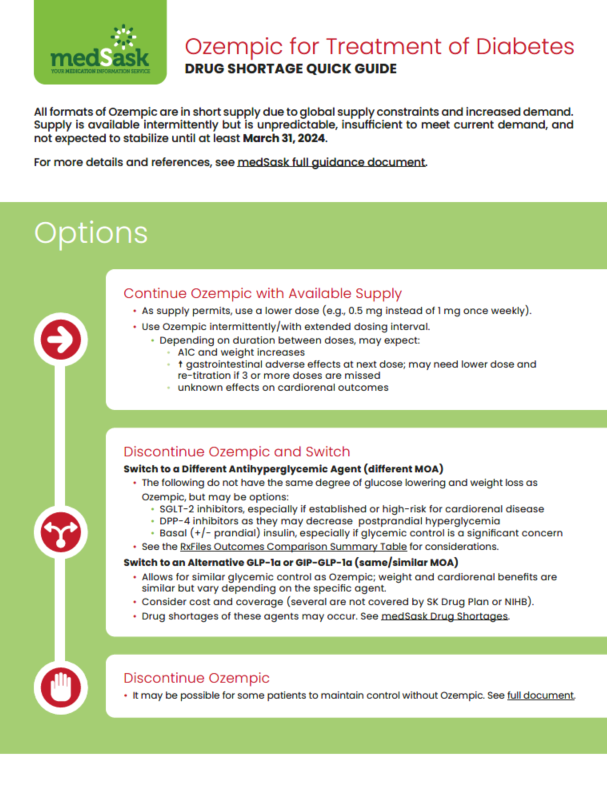
Ozempic for Treatment of Diabetes - Drug Shortage
Ozempic supply is expected to be intermittent and unpredictable until at least March 31, 2024.
Ozempic for Treatment of Diabetes Guides
The Quick Guide contains management options, considerations for choosing alternative agents, and practical tips. See the Full Guidance Document for more detailed information and references.
Management Options
- Continue Ozempic with Available Supply
- As supply permits, use a lower dose (e.g., 0.5 mg instead of 1 mg once weekly).
- Use Ozempic intermittently / with extended dosing interval.
- Depending on duration between doses, may expect:
- A1C and weight increases
- ↑ gastrointestinal adverse effects at next dose; may need lower dose and re-titration if 3 or more doses are missed
- unknown effects on cardiorenal outcomes
- Depending on duration between doses, may expect:
- Switch to a Different Antihyperglycemic Agent
Switch to an Antihyperglycemic Agent from Another Class
- The following agents do not have the same degree of glucose lowering and weight loss as Ozempic, but may be good candidates during the shortage:
- SGLT-2 inhibitors, especially if established or high-risk for cardiorenal disease
- DPP-4 inhibitors as they may decrease postprandial hyperglycemia
- Basal (+/- prandial) insulin, especially if glycemic control is a significant concern
Switch to an Alternative GLP-1 Agonist or GIP-GLP-1 Agonist
- Allows for similar glycemic control as Ozempic; weight and cardiorenal benefits are similar but vary depending on the specific agent.
- Consider cost and coverage (several are not covered by the Saskatchewan Drug Plan or NIHB).
- Drug shortages of these agents may occur. See medSask Drug Shortages
- See full document for approximated equivalent doses and how to switch.
See the Quick Guide or the RxFiles Outcomes Comparison Summary Table for considerations.
- The following agents do not have the same degree of glucose lowering and weight loss as Ozempic, but may be good candidates during the shortage:
- Discontinue Ozempic
- It may be possible for some patients to maintain control without Ozempic. See full document.
Monitoring and Follow Up
- Monitoring
- Glycemic targets
- A1C: every 3 months with therapy adjustment/change
- Self-monitoring of blood glucose: 1 or 2 times per week; increase frequency if using insulin, experiencing signs/symptoms of hypoglycemia, and/or during illness
- Serum creatinine, eGFR
- SGLT-2 inhibitors: serum creatinine increase expected on initiation (up to 25-30%). Reassess if >30%. Obtain baseline, repeat 2 to 4 weeks after initiation, then periodically.
- Other agents: baseline and periodically
- Liver function tests
- SUs, TZDs, repaglinide – baseline and periodically
- DPP-4 inhibitors – baseline
- Volume status, blood pressure
- SGLT-2 inhibitors: periodically; monitor for hypovolemia, hypotension
- Electrolytes
- SGLT-2 inhibitors: within 2-4 weeks of initiation, then periodically; monitor for hypovolemia, renal function (K+)
- Adverse effects
- Metformin: nausea, diarrhea, abdominal discomfort, anorexia, metallic taste, lactic acidosis if hepatic or renal disease. Vitamin B12 deficiency with long-term use
- DPP-4 inhibitors : nasopharyngitis, hypersensitivity reactions, pancreatitis (rare), severe joint pain (rare)
- GIP-GLP-1 agonists: nausea, vomiting diarrhea, injection site reactions, acute pancreatitis (rare)
- GLP-1 agonists: nausea, vomiting, diarrhea, injection site reactions, acute pancreatitis (rare)
- Insulins: hypoglycemia, lipohypertrophy, weight gain, local and systemic hypersensitivity reactions (rare)
- SGLT-2 inhibitors: increased risk of genitourinary infections; reduced intravascular volume resulting in hypotension; hyperkalemia, risk of diabetic ketoacidosis
- SUs, repaglinide: hypoglycemia, weight gain
- TZDs: weight gain, fluid retention, hemodilution; worsening heart failure; macular degeneration; increased risk of fractures and possibly bladder cancer
- Safety
o Sick day management (SADMANS)
o Hypoglycemia
o Ketoacidosis
- Glycemic targets
- Follow Up
- When adjusting medications, follow up within three months.
- Establish a follow-up plan and set triggers when alternative therapies will be considered (e.g., if A1C increases > x%; signs/symptoms of hyperglycemia).
- Assess medication adherence, injection technique/administration, glycemic control, clinical status changes (including renal health and cardiovascular health), adverse effects, and safety.
- If not at glycemic targets:
- Consider dose titration if not at maximum recommended dose (cautions: consider risk of hypoglycemia if applicable; maximum doses of SGLT-2 inhibitors provide little additional A1C lowering compared to lower doses).
- Add another antihyperglycemic agent from a different class, and/or add/intensify insulin regimen.
- Consider referral to diabetes education clinic for assistance with behavioral modifications and goalsetting.
- When adjusting medications, follow up within three months.
End of Shortage
- When Ozempic Returns
- Review therapy with the patient.
- There may not be a need to return to GLP-1 agonist therapy if treatment goals are achieved and patient is satisfied with regimen.
- Re-initiation of GLP-1 agonist therapy:
- Initiate with GLP-1 agonist starting dose unless fewer than three consecutive doses were missed.
- DPP-4 inhibitors should not be used in combination with GLP-1 agonists because the combination provides no additional benefit but increases cost. Ensure these agents are discontinued upon restart of GLP-1 agonist therapy.
- If insulin is continued when GLP-1 agonist therapy is restarted, reduce the dose by 20-30% and adjust.
- Consider adjustment of SU dose based on A1C:
- ≤ 7.5%: stop SU
- 7.6 to 8.5%: reduce dose by 50%
- > 8.5%: maintain current dose
- Review therapy with the patient.
Shortage and Supply Information
Supply of alternatives to Ozempic may also be strained due to increased demand. For information about drug supply:
- medSask Drug Shortages
- Contact medSask by email or phone
- Drug Shortages Canada
Other Resources
- Websites
- RxFiles Diabetes Book
- Diabetes Canada Quick Reference Guide
- Saskatchewan Drug Plan
- Bulletin 861- Information for Pharmacists
- Patient Handout
- Health Canada
- Articles
- Special report: potential strategies for addressing GLP-1 and dual GLP-1/GIP receptor agonist shortages. doi: 10.2337/cd23-0023
- Switching Between GLP‐1 Receptor Agonists in Clinical Practice: Expert Consensus and Practical Guidance. doi: 10.1111/ijcp.13731
- Switching Between Glucagon-Like Peptide-1 Receptor Agonists: Rationale and Practical Guidance. doi: 10.2337/cd19-0100
- Abbreviations
A1C = glycated hemoglobin
DPP-4 = dipeptidyl peptidase-4
eGFR = estimated glomerular filtration rate
GIP-GLP-1 = glucose-dependent insulinotropic polypeptide and glycoprotein-like peptide-1
GLP-1 = glycoprotein-like peptide-1
NIHB = Non-Insured Health Benefits
SGLT-2 = sodium-glucose transporter-2
SU = sulfonylurea
TZD = thiazolidinedione